About a month after I turned 33yo, I got Norwegian citizenship, got my grade for my master’s thesis, and boohoo.. Lost an internal organ. So, this entry is about the latter. About my experience being on the other side of the fence – as a patient, and how it was like to receive specialist care in Norway. These are purely my experiences, my opinions, my observations..
I should actually be very careful when sharing experiences like this, because I’m a nurse and I have the duty to uphold the good image of the healthcare system. But at the same time, I’m also human. There is this thin line that separates my personal life and my career. However, no matter how thin that line is, it still exists and I should be able to tell how it’s like to be a patient. So, I’m sharing this to relay awareness.
So, it all started in November 2022. You see, I really worked hard to lose weight over the past months. I managed to lose around 9kgs through diet and exercise. Then, I realized that my body would hurt whenever I didn’t move. It was weird, but I think it had some effect on what came later.
During the second half of 2022, I started working full-time in the hospital while writing my master’s thesis. There were many nightshifts – 5 in a week, to get a week free later so I could write my thesis. Seriously, all those research studies about how awful it is to work shifts, and what harm it does to your body – all REAL. It was tough to shift back the body rhythm after a week of nightshifts. By the first week of November, I had a flu – slight fever, cough, sore throat.. I still went to work though, ‘coz that’s what we do. You take paracetamol, wear a mask, and show up. The week after the flu, I had severe back pain – I thought I had pneumonia. It was upper back pain, not concentrated on the left or right, but upper. And it radiated towards my shoulders and neck. I have a massage chair at home, so I often go there after work, but the pain didn’t go away. Later on, I was having stomach pain, nausea and vomiting, slimy stool and was burping a lot. I was losing weight. I decided to change my diet and follow a FODMAP diet, which is recommended for people with colon problems. It didn’t really help my case.
Two weeks later, I decided (and finally had the time) to see my GP (or fastlege). He told me that stress was the culprit – you know, considering the nightshifts, the thesis, the job… So, he prescribed anti-nausea Somac (or pantoprazole), to take 1x daily and as necessary, and told me to take it easy. It was Friday. I was a bit disappointed because he based everything on my anamnesis and did not do a stomach check.
I went home, and on Friday night, I was in a horrible state. Same symptoms as described earlier, only severe, and I was puking a lot. Anything I ate, I vomited. That included water, my friend. It was horrible. I thought I puked all that was in my tummy – and the puke was more like yellow fluid. We were going to Sweden in the morning of Saturday to go shopping, but I told my husband that I couldn’t sit still in the car and needed to go to emergency first.

They took my vitals (temp 37.2C, BP 122/78, pulse 73 and SPO2 99%). So, I seemed fine. A urine and blood test was also taken, which turned out positive for leukocytes. My CRP was at <10 at that time. The doctor inspected my tummy and afterwards, I was injected painkiller medication (Voltaren). Hallelujah, it was effective! I was sent away, and my husband and I continued the drive to Sweden.
By Saturday night, the painkiller had worn off and I was back to the previous horrible state. I didn’t manage to get any sleep at all. Same symptoms, plus fever. So, we went back to the emergency ward early Sunday morning – now, they have to take me seriously! I told my inner self. Same procedure: vitals ok (BP 146/88, pulse 74, temp 37.3C, SPO2 100%). CRP now at 16. They took an ultrasound of my tummy and I was told that it was possible I was suffering from gallstones attack, or cholelithiasis. They sent me to the hospital – acute ward. It was 8 am.
The nurse came, took my vitals, left and got busy with another patient. A doctor came, took my anamnesis, and left. Another doctor came and did more checks a little before lunch. That was it. I was there alone, in excruciating pain. The first thing I told the nurse when I arrived was that I wasn’t administered any painkiller in the emergency ward. But I guess it was protocol that patients suffer in pain for them to see what’s up? I puked a couple of times – a substantial amount of yellow fluid. I think I even cried myself a couple of times, feeling abandoned – boohoo.
At 15pm, finally, I was given a vein access and painkiller was administered. It was the first time I had Oxynorm, or oxycodone. I felt light-headed but it literally didn’t have any effect at all. My body still felt like being divided in the middle. I was moved to the surgical ward – awkward, because it’s one of my work wards.






Long story short, I was confined for 5 days. A different doctor came in and out every day. I puked, had fever, and severe stomach and upper back pain. I was administered i.v. fluids and oral antibiotics. The doctors said that most elderly get antibiotics intravenously, but the younger ones usually tolerate oral pills and the symptoms go away. They checked my blood every day, and my CRP peaked at 94, my leukocytes fluctuated from 13, 11, 11 and 7.
Hospital food:


The nights were sleepless, thanks to the neighbor patient snoring her heart out. My husband visited me every day at 5pm (visiting hour), and I’m very thankful for that. I talked to other neighbor patients coming in and out. Some of them had been waiting for cholecystectomy for months that they had to suffer several attacks and get confined in the hospital in the process. One of them, who just had the surgery, said that that it was all good and recommended. She also said something that got stuck with me: Noen smerter må man kunne tåle. (One should be able to tolerate some pain). So, yes, the doctor told me that surgery was the possible cure, after the ultrasound came back positive for cholecystitis (inflammation of the gallbladder) and a 1-cm stone. Slush was also visible.
I thought that getting the surgery (laparoscopically) done at this age would be to my advantage. Besides, my mom just revealed that she had the same experience, was also confined, but she didn’t get any surgery. She was only prescribed pills that would dissolve the stones. Those pills weren’t really popular in Norway, as I was told by the doctor. So, I was put into the waiting list. Upon discharge, the doctor told me that there’s only a couple of months waiting time – meh, that was a lie. 🙂
When I was discharged, I wasn’t really still feeling well. I still have severe pain and nausea. I had to continue the antibiotics at home for 5 more days, and I was prescribed painkiller. Days passed and I still had pain. So, I decided to stop the painkiller. Voila, a couple of days later – I felt much better and was almost back to my normal self. The next couple of weeks, I only ate home-cooked meals. The positive thing about the hospital confinement was that I lost a few more kilograms!
Getting some fresh air and nourishing myself with home-cooked meals:




One of the best things in Norway is free healthcare. Well, you need to pay 15% of medical fees and you get discounts for prescribed medicines, but hospital confinement and surgical procedures are shouldered by the state (or the people’s taxes). However, waiting time can be a huge bummer. I waited months to get in treatment once, for example. It’s also rare to get an appointment with your GP earlier than 2-4 days. Sometimes, it even takes weeks. So, the first schedule for the surgery that I got was in April. That’s 4 months from the hospital confinement, and for some reason, it coincided with the trip to Iceland. So, YOLO, I asked them to change that schedule. I told them that the doctor said 2 months waiting time, not 4. As it turns out, hospital doctors have no say in scheduling surgical procedures. I just accepted what they told me: I would have to wait longer, maybe even after summer, for the next schedule.
But alas, I got the next sched and it was on the first week of June. It also coincided with a holiday, but thankfully, we haven’t booked anything yet. So I made all the necessary arrangements for the surgery (work, work, work). There was a pre-consultation and blood work a couple of days prior the surgery, so it was also carried out. On the day itself, I was so anxious. It was my first time to go under an all-out surgical procedure, although I was told that it’s just a small operation. 2 hours into waiting, I stood up and stretched.. The nurse told me to go back to my assigned seat. Patients came and went. Again, I felt forgotten. No one came to inform me of what’s going on. Other patients were visited by their surgeons and/or the nurses to give information. But to me..nada. At around 12 noon, I couldn’t take it anymore. So I went to the desk and asked what’s going on. They told me that there was an emergency, so there might not be a surgery for me on that day. Lol – was it tough to tell me that earlier? I was told to wait for the surgeon. I was, again, on the verge of crying (oh, what fasting does to the psyche). I told that nurse that I was very thirsty. A few moments later, she came with a pre-op nutritional drink.


The surgeon came after 5 hours of waiting. He looked tired, and he was sorry. I said it’s ok, but that I needed to get a sick leave for that day. I felt disappointed that day, to be honest. I was so anxious, but then, it wasn’t my day.
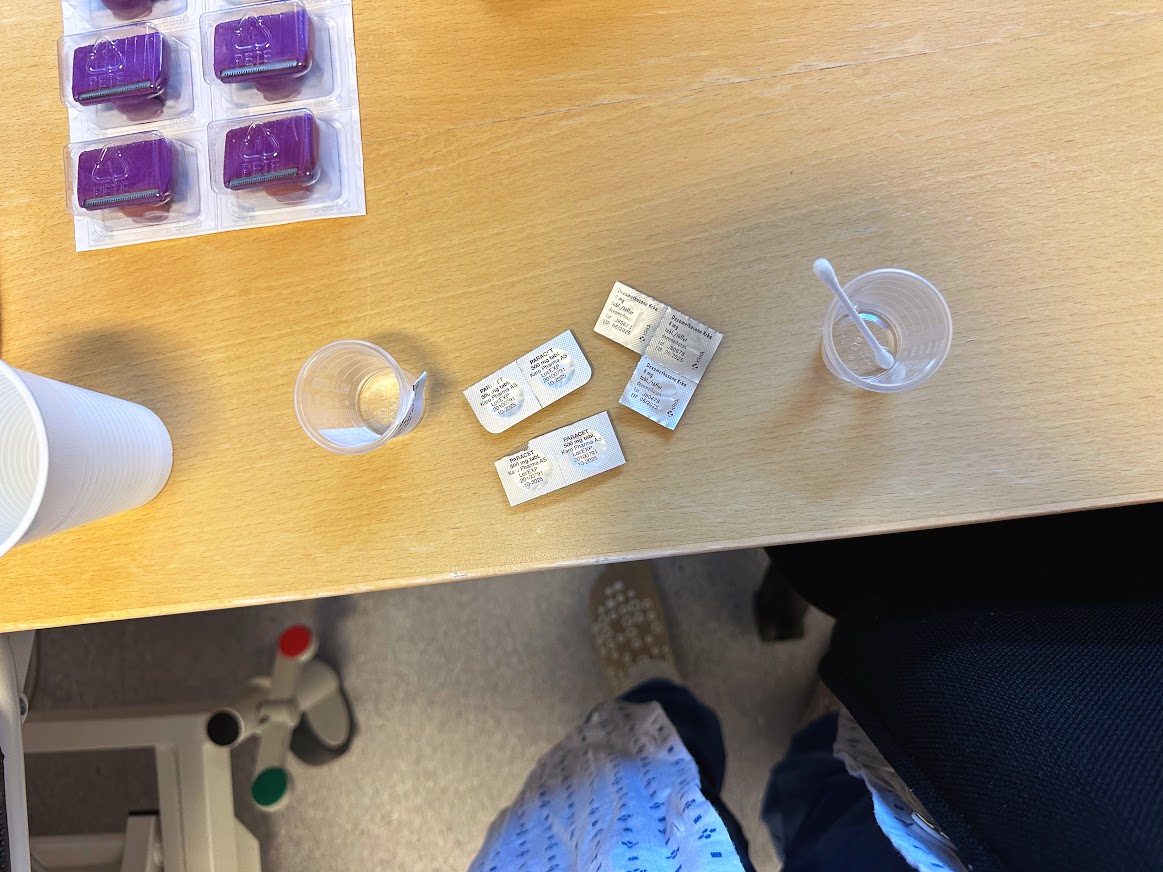
I got the next schedule on June 30. I was put first on the list, so I guess, it was a good sign. The anxiety was still there, but I guess, the expectations were lower. The fasting time was also shorter than last time (where I had empty stomach for around 17 hours). I arrived at 6:50am, and at 7am, I was given the premedication (2g paracetamol and 12 mg dexamethasone). I was told to change and to use klorhexidin to clean my navel. Hehe 🙂


I was so excited that I emptied my bladder 3x. The surgeon came at 7:30 am and discussed the procedure with me. It was text book, but the thing that gave a cling to my ears was: For many, it would feel like having done 100 pushups after waking up. He also mentioned that a breathing tube will be used, so I’d probably get throat irritation after. There will be 4 incisions, and afterwards, I would be moved to the observation ward, and then, the bedpost. I asked if I could be moved to a ward where I don’t work. He said that it’s very possible.
At 8am, I was led to another waiting room with another patient. Then, I was picked up by the anesthetist and the surgical nurse. I was led to the surgical room, put on a surgical cap, and asked to make myself comfortable on the table. I felt really well taken care of! I got i.v. access and was connected to a 500 ml NaCl infusion. The surgical nurse told me that she was going to go through the procedure checklist, while administering air through a thick mask. She told me to breathe deeply twice – and I guess that was it. I was out.
Later on, someone was calling my name (the Norwegian pronunciation). Maerose, Maerose! Operasjonen din var ferdig! (Your operation was over). That person shook me awake, and then left me to the care of the nurse. I asked where I was, well – I was now in the observation post. It was 9:30 am. The nurse there was also very accommodating and pleasant. She gave me water, juice, and Oxynorm (oxycodone: i.v. and capsule). I still had an NaCl i.v. drip. I was super thirsty. The nurse said I might be dehydrated. I drank like 5 cups of water. And oh! I wa given a vial containing my gall bladder stones! Two of them.. Guess they grew and multiplied since November.. It was now around 1,5 cms in diameter.
I asked the nurse if she could tell me what medications were used for the operation. So, it was a mix of Propofol (anesthesia), Fentanyl (painkiller), and some NSAID. She said she’d go back with the list, but then, she went for lunch and I guess, forgot all about it. It’s okay though.
I spent precisely 2 hours in the observation ward. I mobilized myself twice, sitting up on the bedside, first with the help of the nurse, and then, alone. I did have pain in my tummy, especially in the navel region. The nurse scanned my bladder for around 90 ml, so I was told I should drink some more. I was also administered Oxynorm i.v. again to relieve more pain. I had one episode with nausea, but the nurse was quick to give me a vomit bag and was about to administer Afipran i.v. (anti-nausea), but it passed, so there was no need for it in the end.
It was painful to get out of bed, but I’ve learned techniques from my work, so it went fine. It was also painful to cough and laugh, so the nurse gave me the taped towel cube: to hug while I sneeze, cough, laugh. Then, I was moved to the bed post at around 11:30 am.
The first nurse at the bed post was also nice. She helped me mobilize myself, but I only managed a short distance. I was still pain-relieved, but the nurse said that the pain caused by the carbon dioxide often comes later on (and boy, was she right). I had a tough time urinating while in the bed post, and I had zero appetite. I napped, and drank a lot of water. I tried 3x before finally getting some water out of my system. Very little, not much. I had 3 different nurses during at the bedpost. The first nurse showed my stones to her colleagues, and I was told that they were fascinated. During my short stay there, I only received 1g paracetamol for the pain, and it was okay.



The surgeon came around 2pm and told me that everything went fine. He prescribed some pain reliever (Tramadol), to be used as necessary. I had no plans of using it though. I know how mean Tramadol can be to the kidneys, how it can cause and maybe worsen urine retention. Besides, I was worried about painkiller abstinence symptoms afterwards. You know, when you feel more pain upon stopping. The surgeon said that I could go home when I’m ready, or stay a night in the hospital. I should just have someone with me for the first 24 hours. I wanted to go home; I had a bad experience sleeping in the hospital from the last confinement. And I always feel that recovery from home is best. I knew the procedure prior to going home, and I guess I knew what to do if things don’t go well at home. I asked the nurse to scan my bladder before leaving (around 100 ml residual urine), and to give me some bandages so I could tend to my wound at home. There were already blood stains on the bandages, but I’m not changing them before 2-3 days.
My husband picked me up from the hospital at around 15:30 pm. I bought some anti-scar bandages, some mild laxatives (should I take T capsules), a box of paracetamol, and some honey drops for my sore throat from the breathing tube from the hospital drugstore. I also picked up the T capsules. All in all, I spent ca 500 kr for everything.
The rest of the day went okay – I mobilize myself and I managed to go and pee now. I also had some watermelon and half a banana. And then, at around 7pm, the painkiller wore off and I had a sudden pain in my tummy. I couldn’t breathe and couldn’t sit up from bed! I was crying and asking for help. Lols. Although I knew that it was caused by the gas. I also had the shoulder pain now. Scared of not being able to sit back up, I decided to sleep sitting up on the first night. My back hurts a little bit, but at least, I didn’t have to struggle. The bloating was real! I also decided to take a capsule of T and 500 mg of Paracet, but the pain was still there. So, I’ll try just paracetamol tomorrow.
It’s 4 am now, couldn’t sleep. My cats have been so sweet. We think that they knew I wasn’t ok. Missy slept beside me the whole night. Well, let’s see how I’ll be recovering from my first all-out surgery 🙂 I also got a B for my master’s thesis, which isn’t that bad. So, all in all, I’m happy and blessed! Happy weekend!
#spreadloveandpositivevibes
ALL PHOTOS AND VIDEOS ON THIS BLOG ENTRY ARE MINE. 🙂 Cheers!
PS. If you’re as curious as to how laparoscopic cholecystectomy is done, here’s a Youtube video for you (credits to the owner of the video; patient not me):





Leave a comment